-
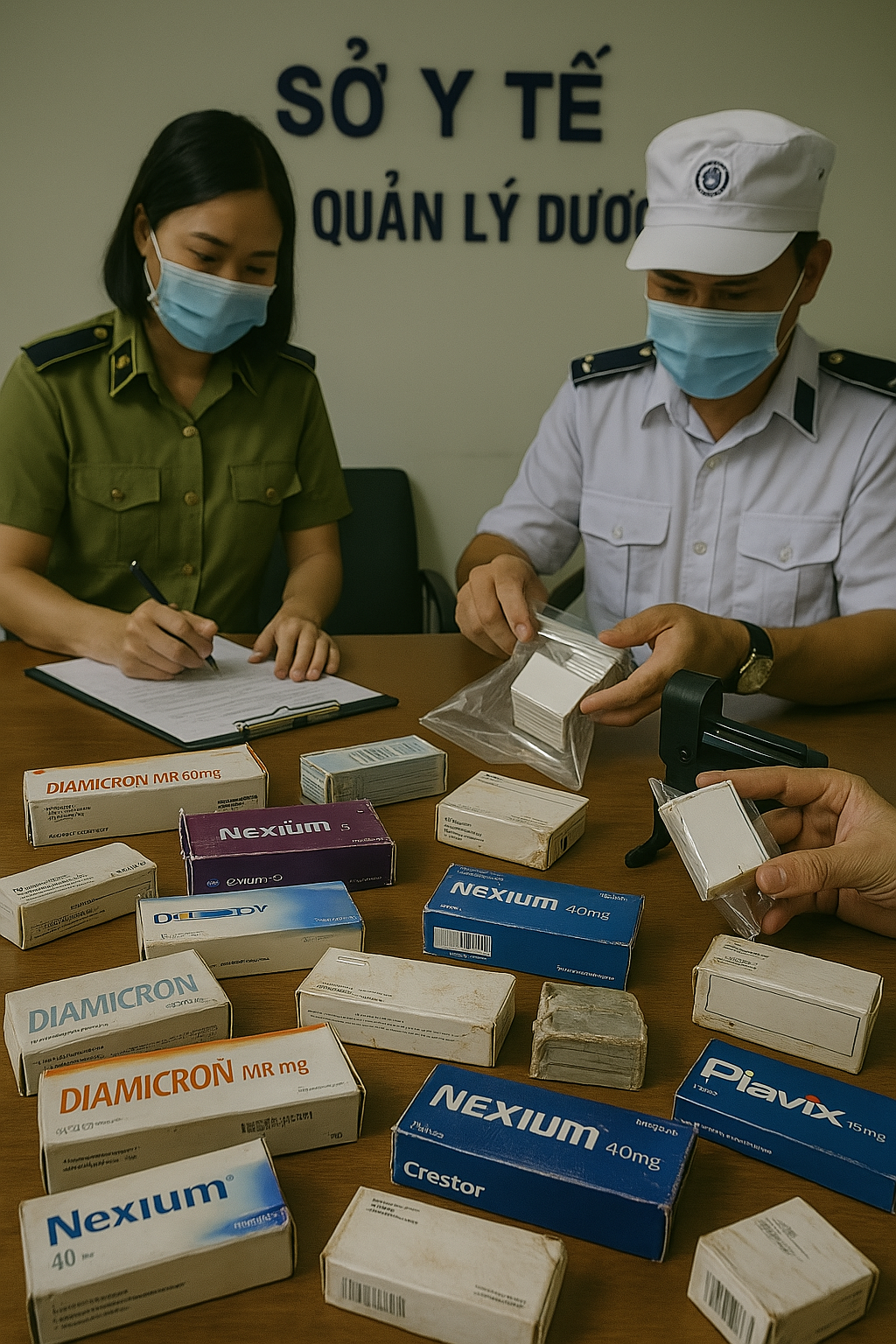
 Tăng cường xử lý tổ chức, cá nhân sản xuất, buôn bán thuốc chữa bệnh và sữa giả
Tăng cường xử lý tổ chức, cá nhân sản xuất, buôn bán thuốc chữa bệnh và sữa giả -
 [HƯỚNG DẪN] Đăng ký SmartCA từ ứng dụng VNeID
[HƯỚNG DẪN] Đăng ký SmartCA từ ứng dụng VNeID -
 CHƯƠNG TRÌNH LỄ KỶ NIỆM 70 NĂM NGÀY THẦY THUỐC VIỆT NAM - TTVH NT AN GIANG - VĐ NGỌC PHƯƠNG NAM
CHƯƠNG TRÌNH LỄ KỶ NIỆM 70 NĂM NGÀY THẦY THUỐC VIỆT NAM - TTVH NT AN GIANG - VĐ NGỌC PHƯƠNG NAM -
 HTV9 | Hội Nghị Đẩy Mạnh Chuyển Đổi Số và Đồng Bộ Dữ Liệu trong Y Tế & Lao Động
HTV9 | Hội Nghị Đẩy Mạnh Chuyển Đổi Số và Đồng Bộ Dữ Liệu trong Y Tế & Lao Động -
 Dấu ấn công tác y tế 2024: “ĐOÀN KẾT, KỶ CƯƠNG, NÊU GƯƠNG, TRÁCH NHIỆM, HIỆU QUẢ”
Dấu ấn công tác y tế 2024: “ĐOÀN KẾT, KỶ CƯƠNG, NÊU GƯƠNG, TRÁCH NHIỆM, HIỆU QUẢ” -
 Sức khỏe và cuộc sống (24-10-2024)
Sức khỏe và cuộc sống (24-10-2024) -
 Tọa đàm Bệnh lý đột quỵ thực trạng tại An Giang và những tiến bộ trong tiếp cận, điều trị hiện nay
Tọa đàm Bệnh lý đột quỵ thực trạng tại An Giang và những tiến bộ trong tiếp cận, điều trị hiện nay -
 TUẦN LỄ THẾ GIỚI NUÔI CON BẰNG SỮA MẸ (1 – 7/8/2024)
TUẦN LỄ THẾ GIỚI NUÔI CON BẰNG SỮA MẸ (1 – 7/8/2024) -
 Thông điệp phòng, chống bệnh bạch hầu
Thông điệp phòng, chống bệnh bạch hầu -
 Những điểm mới trong Luật Khám bệnh, chữa bệnh (sửa đổi) năm 2023
Những điểm mới trong Luật Khám bệnh, chữa bệnh (sửa đổi) năm 2023 -
 Bệnh viện Đa khoa Y học cổ truyền - Phục hồi chức năng tỉnh An Giang
Bệnh viện Đa khoa Y học cổ truyền - Phục hồi chức năng tỉnh An Giang -
 Cách xử trí người bị say nắng, say nóng
Cách xử trí người bị say nắng, say nóng -
 Khuyến cáo phòng bệnh ho gà
Khuyến cáo phòng bệnh ho gà -
 Thông điệp phòng bệnh dại
Thông điệp phòng bệnh dại -
 AN GIANG: BỆNH VIỆN Y DƯỢC CỔ TRUYỀN - PHỤC HỒI CHỨC NĂNG CHÍNH THỨC HOẠT ĐỘNG
AN GIANG: BỆNH VIỆN Y DƯỢC CỔ TRUYỀN - PHỤC HỒI CHỨC NĂNG CHÍNH THỨC HOẠT ĐỘNG


.jpg)
.png)

.jpg)
.jpg)
-6-25.png)
.png)